With Advances in Cancer Immunotherapy, Scientists Discuss Need to Develop New Mouse Models
, by NCI Staff
About 50 researchers met this fall to exchange ideas about how mouse models could be used to develop and improve new treatments that harness the immune system against cancer.
The meeting, held at NCI’s Shady Grove campus on September 18–19, highlighted the challenges and opportunities associated with using cancer models to conduct research on immunotherapies.
As more patients with cancer have received immunotherapies, some of the limitations of these treatments have become clear. For instance, only some patients respond to them, and the treatments can have potentially serious side effects caused by the stimulation of immune responses.
“Our goals were to assess the state of the science of immunotherapy and to discuss what questions we can ask using existing mouse models and what new models are needed to ask other questions,” said Dinah Singer, Ph.D., director of NCI’s Division of Cancer Biology (DCB).
DCB co-sponsored the meeting with the Jackson Laboratory Cancer Center and the National Institute of Allergy and Infectious Diseases (NIAID), another component of NIH. Participants included experts from fields such as cancer biology, immunology, clinical research, and bioinformatics.
“We were trying to get researchers to help us understand which areas of model improvement would be important for NCI to fund,” said Cheryl Marks, Ph.D., of DCB. “We didn’t expect to solve every problem at the workshop, but we did expose some areas where we might delve deeper into the science of modeling.”
For example, participants agreed that additional mouse models will likely be needed to study interactions between the immune system and tumors, and to identify biomarkers associated with immune responses.
“Model systems are critical to answering these kinds of questions and to continued progress in immunotherapy,” said Edison Liu, M.D., of The Jackson Laboratory. “Everybody at the meeting believes this.”
Mouse Models Help Demonstrate the Potential of Immunotherapies
Mouse models have been instrumental in the development of some types of immunotherapy, several presenters noted at the start of the meeting.
A landmark 1996 study used mouse models to show that targeting certain checkpoint proteins on immune cells could release the “brakes” on the immune system, enhancing the ability of immune cells to attack tumors.
That research, led by James Allison, Ph.D., then at the University of California, Berkeley, laid the foundation for the development of a new class of drugs known as immune checkpoint inhibitors. These drugs have benefited a growing number of patients with cancer, including some who had run out of treatment options.
And the Food and Drug Administration (FDA) recently approved two treatments known as CAR T-cell therapies, which use genetically engineered immune cells collected from patients to attack their cancers. Mouse models also played an important role in the development of this approach.
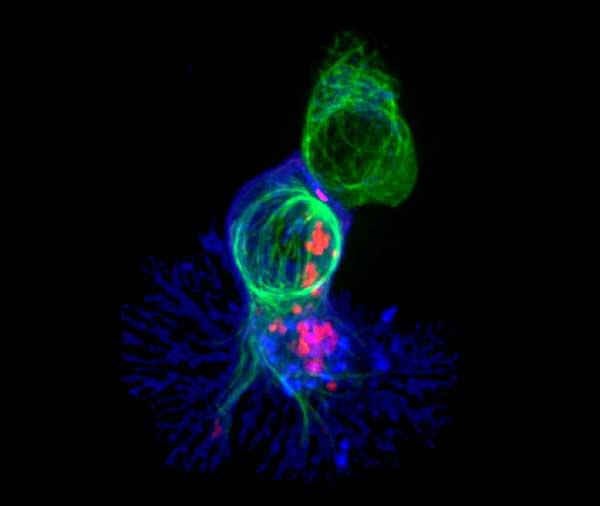
Cancer models, including genetically engineered mice and cellular systems such as organoids, allow researchers to study dynamic interactions between tumors and the immune system in ways that are not possible in clinical studies.
There are only so many experiments that researchers can do in humans because of the costs, ethical questions, and time involved, noted Ronald Germain, M.D., Ph.D., chief of the Laboratory of Systems Biology at NIAID.
“Although there’s a debate about how relevant mouse models are to human tumors, the models clearly are valuable if used judiciously,” Dr. Germain said. “It’s important to understand the limitations of a model and to consider them when interpreting the results of experiments.”
A Better Understanding of the Biology
A consensus among the researchers emerged early in the meeting: For continued progress in immunotherapies, a better understanding of the biology of immune cells and other components of the immune system is needed.
One of the challenges for the field, noted Dr. Liu, comes from trying to model the interactions of two distinct biological systems—the immune system and the tumor in its environment.
“The framework here is [biological] complexity, and we have to be able to model it,” he continued. “We’re talking about developing preclinical systems that will allow us to home in on certain questions as we move into human trials.”
In the past, mouse models have tended to be what researchers call monochromatic. For example, a mouse might carry a single genetic mutation that primarily affects one type of tissue. But this approach may not be adequate for modeling the complexity associated with an immune response and the variety of genetic and other factors that may influence such responses.
“We need to generate models that represent the combinations of oncogenes and genes involved in generating immune responses against cancer,” said Dr. Liu.
The severe side effects that can occur with immunotherapies were also discussed at the meeting. Participants said that being able to predict which side effects may occur in patients is important.
Toxicity studies often use a single type of mouse model, but using multiple strains or panels of mice is likely to be more informative, participants noted. Similarly, biomarkers are needed to help identify patients at particular risk for certain side effects as well as to identify patients who are likely to respond to a given treatment.
The Importance of Well-Characterized Models
To make progress on biomarkers, for example, researchers will need detailed knowledge about the biology of the mouse models they are using, some participants said. This includes knowing how a mouse model was engineered and the potential biological effects of these changes.
“The characterization of the mouse was a very important topic at the meeting,” said Mariam Eljanne, Ph.D., of DCB. Some participants also highlighted the need to standardize research protocols and reagents in experiments with mouse models.
“If there’s one thing NCI hears from researchers, it’s the importance of having reliable reagents,” said Dr. Marks. “They put a lot of time and money into developing reagents they can trust. If researchers aren’t using standard reagents or validated reagents, then the results of their experiments might not be reproducible.”
Many of the checkpoint inhibitors, for example, are a type of biological drug known as a monoclonal antibody.
“These antibodies are complex, and how the components of each antibody are constructed seems to affect the immune response,” said Dr. Liu. “We’re still trying to figure out the relationship between the antibodies’ structures and how that affects their activity.”
A related issue is that immunotherapy products can vary, for reasons that are not always clear, even to the people producing them. When researchers at different institutions are evaluating a particular treatment, they need “validated therapeutic tools that would ensure that everyone is testing the same drug,” said Dr. Liu.
Selecting the Appropriate Mouse Models for Experiments
Many participants stressed the importance of selecting the appropriate model for a given experiment. In the past, they noted, some researchers have used models to investigate questions that the models were not designed to answer. Dr. Liu also noted that the field has relied too much on certain mouse models.
In recent years, the development of new xenograft mouse models derived from patient specimens was “a response to the questionable translational value of earlier and widely used human cell line xenografts in mice,” added Dr. Marks.
The introduction of new technologies, such as the genome-editing tooRemoved broken link per broken link report. l CRISPR, has increased the number and variety of mouse models of cancer, suggesting that it may be more important than ever for researchers to select the most appropriate models.
The Power of Working across Disciplines
Collaboration was a theme of the meeting, which brought together researchers with very different perspectives who could contribute to discussions about the problems in the field.
NCI and NIAID have partnered to create the new Center for Advanced Tissue Imaging, or CAT-I, which could facilitate studies designed to ask why some patients and not others respond to immunotherapies and other treatments.
“The partnership between NCI and NIAID is valuable because it brings together individuals with expertise on tumors and on the basic principles of how the immune system works,” said Dr. Germain. “It applies the power of the biomedical establishment to the problem.”
“We need to be smarter in how we use the models,” said Dr. Germain. “You can’t just pick any mouse with a transplanted tumor off the shelf and expect it to answer all of your questions.”
There were discussions at the meeting about two ways the field could help researchers find and select the appropriate mouse models: characterizing the molecular and genetic features of the models, and making this information easily accessible online.
The Oncology Models Forum
Toward this end, NCI is developing the Oncology Models Forum, an online resource for selecting cancer research models. This platform contains data-analysis tools, shared data sets, and a discussion forum to help researchers comprehensively understand different cell- and mammalian-based models.
“The idea is that when researchers need a mouse [model], they can go online and find one that corresponds to the experiments they want to do,” said Dr. Eljanne.
In the meantime, Dr. Eljanne added, models for cancer are constantly getting better as researchers work to improve existing models and develop new ones.
Dr. Liu agreed. “We have the expertise—and just as important, we have the will in the community—to expand the range of mouse models,” he said. “But it will require investment, and it will require coordination.”