More Evidence that Ruxolitinib Benefits Some Patients with Graft-Versus-Host Disease
, by NCI Staff
Patients with blood cancers who develop graft-versus-host disease (GVHD) within the first few months after receiving a stem cell transplant and don’t respond to steroids are more likely to respond to the drug ruxolitinib (Jakafi) than to other treatments, according to results from a large clinical trial.
The findings are from the first randomized clinical trial of a treatment for GVHD to yield positive results. And the study confirms findings from a smaller trial that, in 2019, led to the approval of ruxolitinib by the Food and Drug Administration (FDA) for some patients with GVHD.
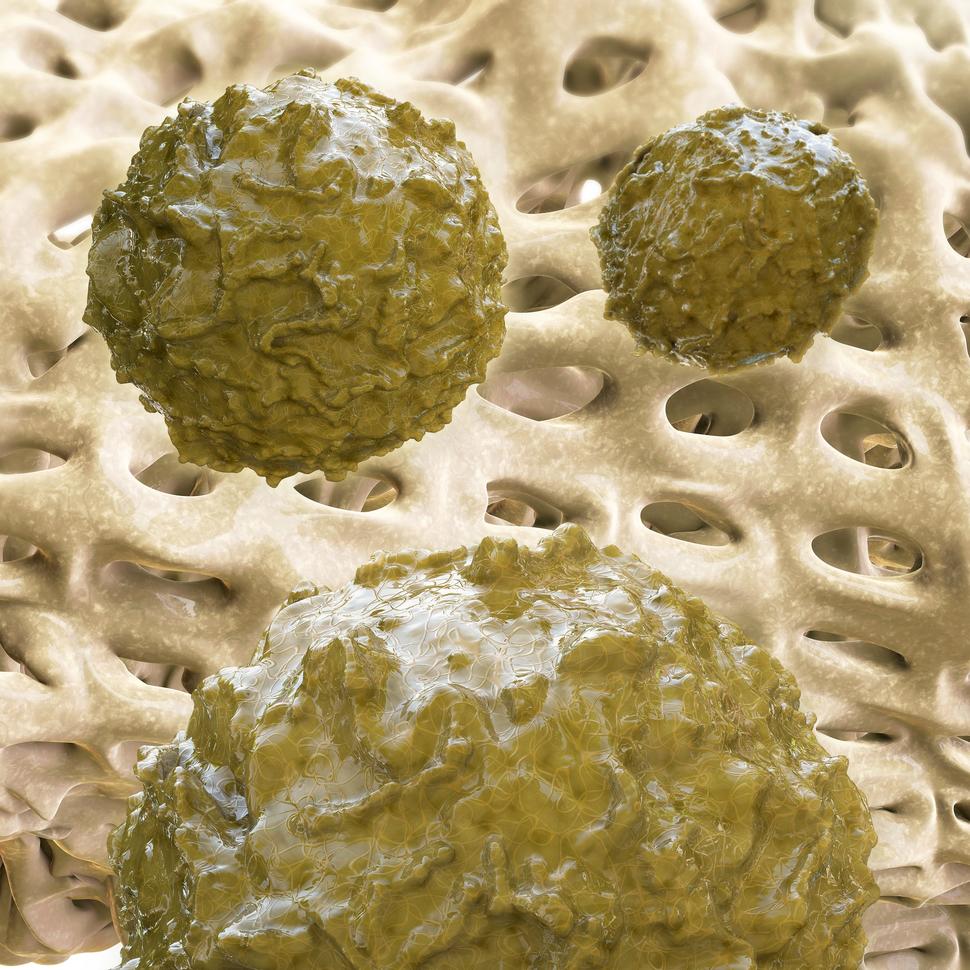
Both trials tested the drug in patients with a form of the disease called steroid-refractory acute GVHD. In these patients, GVHD develops within the first weeks and months after a transplant of stem cells from a healthy donor, also known as an allogeneic stem cell transplant, and the disease does not respond to steroids.
During a transplant, the donor’s healthy stem cells replace the patient’s own cells that have been damaged by radiation therapy or chemotherapy. But in some patients who receive transplants, the donated cells attack the recipient’s cells, causing damage to the recipient’s tissues and organs, which can lead to GVHD. Symptoms of the disease include a widespread rash, diarrhea, and liver damage.
In the new trial, called REACH2, patients received either ruxolitinib or one of nine commonly used treatments for steroid-refractory acute GVHD (control group). After 28 days of treatment, more patients receiving ruxolitinib had a complete or partial response, compared with patients in the control group (62% versus 39%).
This difference in the response rates persisted through 56 days of treatment, and the side effects were similar in the two groups, Robert Zeiser, M.D., of the University Medical Center Freiburg, Germany, and his colleagues reported in the New England Journal of Medicine (NEJM) on April 22.
“This trial demonstrates that ruxolitinib is a new standard treatment for patients with steroid-refractory acute GVHD,” said Steven Pavletic, M.D., of the Immune Deficiency Cellular Therapy Program in NCI’s Center for Cancer Research, who was not involved in the trial.
“The results are very compelling because the drug was tested not against a placebo but against the best available treatments,” he added.
The First Successful Randomized Clinical Trial in GVHD
Between 30% and 50% of patients who have an allogeneic stem cell transplant develop acute GVHD. Steroids are effective for treating GVHD in only about half of all patients, and GVHD can be fatal in patients for whom steroids are not effective or who have a relapse, Dr. Pavletic noted.
Ruxolitinib, a targeted therapy that patients take as a pill, inhibits two proteins, JAK1 and JAK2, that are thought to play a role in GVHD. Blocking these proteins may lead to a reduction in inflammation that is associated with the disease, according to the researchers.
Ruxolitinib “appears to be a relatively specific drug” that may not interact with many molecules other than JAK1 and JAK2, wrote Nelson Chao, M.D., of the Duke University Medical School in a commentary accompanying the study in NEJM. This specificity could contribute to the limited side effects observed in the patients receiving the drug.
Novartis, the maker of ruxolitinib, funded the randomized trial, which was conducted at sites around the world.
The percentage of patients with a complete response (the disappearance of all signs of the disease) was 34% (53 patients) in the ruxolitinib group and 19% (30 patients) in the control group, the researchers reported. The median overall survival (the length of time that half of the patients in a treatment group are still alive) was 11.1 months in the ruxolitinib group and 6.5 months in the control group.
“We need to see if the improved response rate translates into improved overall survival,” said Dr. Zeiser. “Therefore, a long-term follow-up study is needed.”
He added: “It was important to see that there were no unexpected side effects in the group of 150 patients receiving ruxolitinib, and that the drug was well tolerated by patients.”
The most common side effects up to day 28 were thrombocytopenia (in 33% of the ruxolitinib group and 18% in the control group), anemia (30% and 28%, respectively), and cytomegalovirus (CMV) infection (26% and 21%).
Complications from CMV infections “are a major medical problem after allogeneic stem cell transplantation,” said Dr. Zeiser, who noted that if the problem is not treated patients can develop CMV-related pneumonia or eye infections.
Dr. Zeiser had been expecting higher rates of CMV infection in the ruxolitinib group, but the rates were similar in the two groups. “The observation that ruxolitinib did not increase infectious complications is a major plus in terms of the use of the drug,” he said.
In his commentary, Dr. Chao agreed that the CMV results were interesting but cautioned that the follow-up time for patients was short and longer follow up is needed to assess whether the lack of increase in CMV infection remains the case.
Translating Basic Research into New Treatments
Dr. Zeiser and his colleagues designed the trial to compare ruxolitinib with any of nine commonly used treatments for steroid-refractory acute GVHD because, prior to ruxolitinib, there was no standard treatment for this disease.
Now, however, researchers have begun to test many drugs for GVHD that could have similar effects as JAK inhibitors, noted Dr. Pavletic. “This is a very active area of research.”
The groundwork for the current research activity, he explained, was laid during scientific conferences held at the NIH in 2005 and in 2014 that helped to establish criteria for conducting clinical trials in patients with GVHD.
The REACH2 results “show that advances in our understanding of the biology of the disease can be translated into improved therapies for patients,” said Dr. Pavletic.
“But this trial is not the end of the story,” Dr. Pavletic added. “Ruxolitinib is not effective for all patients, and the field desperately needs good biomarkers to know when to intervene.”
Researchers are also testing ruxolitinib in patients with chronic GVHD, which can develop a few months after a stem cell transplant. “We are eager to see those results,” Dr. Pavletic said. (In 2017, ibrutinib (Imbruvica) became the first drug approved by FDA-to treat chronic GVHD.)
Dr. Zeiser expects that future studies will evaluate the potential for using ruxolitinib rather than steroids as the initial treatment for chronic GVHD. In addition, he added, “we’d like to see whether therapies could be used in combination with ruxolitinib to further increase its effectiveness.”