Will This Cancer Metastasize? Check Its “Stickiness”
, by Melissa Madden
Scientists have developed a device that may help oncologists make better decisions about how to treat patients with cancer that hasn’t yet spread to other parts of their body. The device measures the “stickiness” of cancer cells in tumor samples to determine how likely the cells are to escape from the tumor and travel, or metastasize, to other organs.
In experiments in mice, they showed that different levels of stickiness could predict if a cancer would metastasize. And in experiments using human tissue samples, they showed that healthy breast tissue was very sticky, while tissue from advanced tumors was far less sticky.
Results from the study, which was funded in part by NCI, were published March 25 in Cell Reports.
Although they stressed that larger studies are needed, the researchers believe the device could potentially help doctors make more informed treatment choices for their patients with breast cancer, including those diagnosed with ductal carcinoma in situ (DCIS), or what is sometimes called stage 0 cancer.
“The hope with this device is that we'll be able to say to patients,‘You're on the lower side of this metastatic risk spectrum’ or ‘You're at a higher risk, so we suggest a different treatment plan,’” said the study’s senior investigator, Adam J. Engler, Ph.D., a professor of bioengineering at the University of California (UC) San Diego. “We're not there yet. But the data is at least pointing in that direction.”
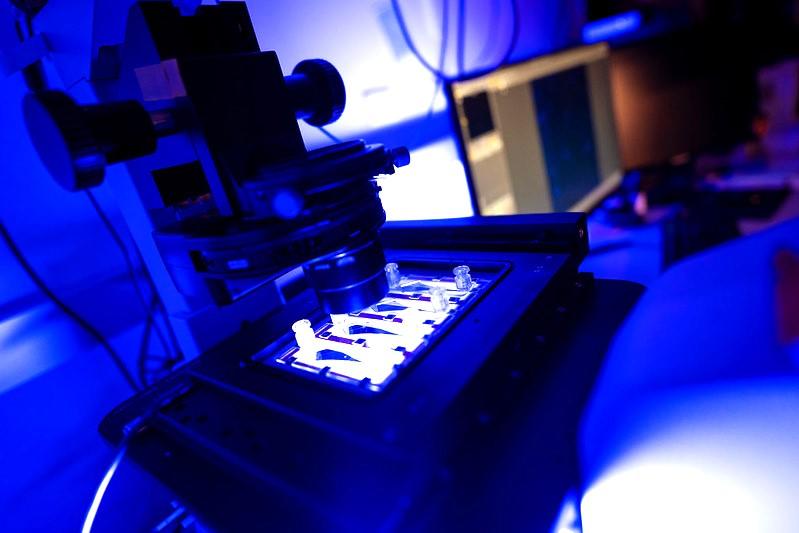
Called a microfluidic device, it uses fluids to push cells from surgically removed tumor samples through chambers lined with a biological material that helps tumors adhere and maintain their structure. The device helps sort the cells by how readily they cling to the chamber walls.
According to Eric Johnson Chavarria, Ph.D., of NCI’s Physical Sciences – Oncology Network, the device takes advantage of cancer cells’ physical properties to identify their potential for seeding new tumors much differently than existing methods.
Additional research should test how well it works across different cancer types and other variables, said Dr. Johnson Chavarria, who was not involved in the study. But the approach, he added, has promise.
“It’s another potential tool that clinicians could use to personalize treatment.”
What is cell adhesion and tumor cell “stickiness”?
All cells have molecules that, like the mortar used to join together bricks in a wall, allow them to adhere to each other and construct the tissue that forms the body’s organs. These same molecules also allow cancer cells to adhere to other cells to form tumors.
A critical step in metastasis is when cancer cells break away from a tumor and slip into the bloodstream or lymphatic system. Metastatic tumors form if any of those cells can find a hospitable location in another part of the body to settle in and start growing again.
Since 2017, the UC San Diego team has been studying how cancer cells break away from tumors and how to physically identify those cells most likely to spread elsewhere in the body.
Some existing methods for assessing tumor aggressiveness—including its potential to spread—rely in part on cancer cells’ physical characteristics, such as how they look under a microscope (e.g., their grade).
Dr. Engler and his colleagues wondered if they could fashion a device that provided a more precise snapshot of this so-called metastatic potential than existing methods.
Different cells, different adhesion
The device, Dr. Engler explained, attempts to mimic some of the physical aspects of tumors, including incorporating a protein called fibronectin, an important component in tumors' adhesion infrastructure. It measures how cells react to what's called fluid shear stress, akin to how a river current can test how securely boats are tied to shore.
When the researchers seeded tumors in mice using cancer cells that the device showed were particularly sticky, far fewer metastases formed in the lungs than when they seeded tumors using cancer cells that were far less sticky.
They then used the device to test human tissue samples taken from 16 women, including from normal breast tissue; DCIS, which is not considered to be invasive; and invasive breast tumors. The cells in normal breast tissue were very sticky, they reported, while cells from the invasive breast tumors were much less adherent.
Madison Kane, the study’s lead researcher and Ph.D. student in bioengineering, said the team was surprised by the different levels of stickiness they saw in the DCIS samples.
Right now, there are no accurate ways of predicting whether DCIS is aggressive and, if left untreated, will eventually start to invade into the breast and potentially spread. Despite the low risk of DCIS becoming invasive, because it can’t be determined whether it will progress to full-blown cancer, most women diagnosed with DCIS get some form of treatment.
Their device, Ms. Kane said, could be used to help identify women with DCIS that has a strong likelihood of becoming invasive and should be treated and women who are at low risk and can forego treatment.
Over the next 5 years, the research team plans to conduct studies testing the device in women with DCIS to get a better understanding of its potential to help guide treatment decisions.
They’re also testing the approach in lung and prostate cancer to determine if this concept might apply to other solid tumors.
“There’s no good universal marker for metastasis,” said Dr. Engler. His team believes that physical features like adhesion could potentially be the first.