Alzheimer’s-Linked Protein May Help Melanoma Spread to Brain
, by Sharon Reynolds
A protein called amyloid beta is infamous as a likely contributor to the development of Alzheimer’s disease. Clumps of it, called plaques, are found throughout the brains of people who develop the cognitive symptoms of Alzheimer’s.
And now, results from a new study in mice by NCI-funded researchers, published March 9 in Cancer Discovery, suggest that amyloid beta also plays a role in the spread (metastasis) of melanoma to the brain. The researchers found that melanoma cells that travel to the brain produce their own supply of amyloid beta and that this protein is necessary for their survival.
They also showed how amyloid beta achieves this feat: by tamping down the body’s normal immune response against cancer cells that make it into the brain. In fending off the immune response, the protein buys the cancer cells time to grow into full-fledged tumors.
Treating the mice with drugs that block the protein greatly reduced melanoma cells’ ability to survive in the brain. These results, the researchers said, raise the intriguing possibility of using drugs developed to treat Alzheimer’s to slow or stop melanoma from spreading to the brain.
Other research groups have also found intriguing connections between cancer that has spread to the brain and neurodegenerative disorders such as Parkinson’s disease, explained Eva Hernando-Monge, Ph.D., of NYU Grossman School of Medicine, who led the new study.
“So we’re trying to understand if [these connections] might present new treatment opportunities,” Dr. Hernando-Monge said.
Tumor cells with an affinity for the brain
Among all cancer types, melanoma is especially likely to spread to the brain. Studies estimate that between 40% to 75% of people whose melanoma spreads will end up with one or more brain metastases. The symptoms of these tumors—which can include seizures, vision and hearing problems, and difficulty thinking and remembering—can be devastating.
“A cancer diagnosis is often a traumatic event, inducing a major lifestyle disruption,” said Brunilde Gril, Ph.D., of NCI’s Division of Cancer Biology, who was not involved with the study. “Brain metastases, affecting cognitive functions, touch the identity and sense of self of the person, adding another layer of emotional and functional challenges.”
Currently, there are no therapies to prevent melanoma from taking hold in the brain. Clinical trials of immunotherapies for advanced melanoma have shown some success in shrinking brain metastases, said Dr. Hernando-Monge. “They work to a certain extent. There’s some reduction in the [size of the] tumors,” but these responses don’t last, she explained.
Her team has been studying the mechanisms that cancer cells use to spread to and thrive in the brain. For this study, the team started with a technique called unbiased proteomics analysis. This approach makes it possible to look at the complete set of proteins produced by cells, without making any assumptions in advance about what will be found.
Using this approach, the researchers compared samples from melanoma that had spread to other parts of the body, such as the lymph nodes of lungs, with samples from the same patients’ brain metastases.
The comparison showed that the cells taken from the brain had different patterns of expression of proteins that are linked to neurodegenerative diseases, including Alzheimer’s, Parkinson’s, and Huntington’s diseases. These included proteins known to be involved in amyloid beta production.
Quieting the immune response in the brain
The team next performed a series of experiments using cancer cells that could and couldn’t produce amyloid beta. The results, including from tests in mice, seemed to confirm that the melanoma cells could spread to other organs without the protein but that it was needed for the cells to establish tumors in the brain.
In another set of mouse experiments that tracked the timeline of melanoma metastasis to the brain, the team found that individual melanoma cells lacking amyloid beta could spread to the brain and survive there for about a week. But they didn’t grow into larger metastatic tumors.
To reach and colonize the brain, cancer cells need to overcome several hostile environments, explained Dr. Gril. The cells start their journey by leaving the primary tumor. They then need to survive in the blood stream, cross a structure known as the blood–brain barrier, and then successfully incorporate themselves among other brain cells to grow as a secondary tumor.
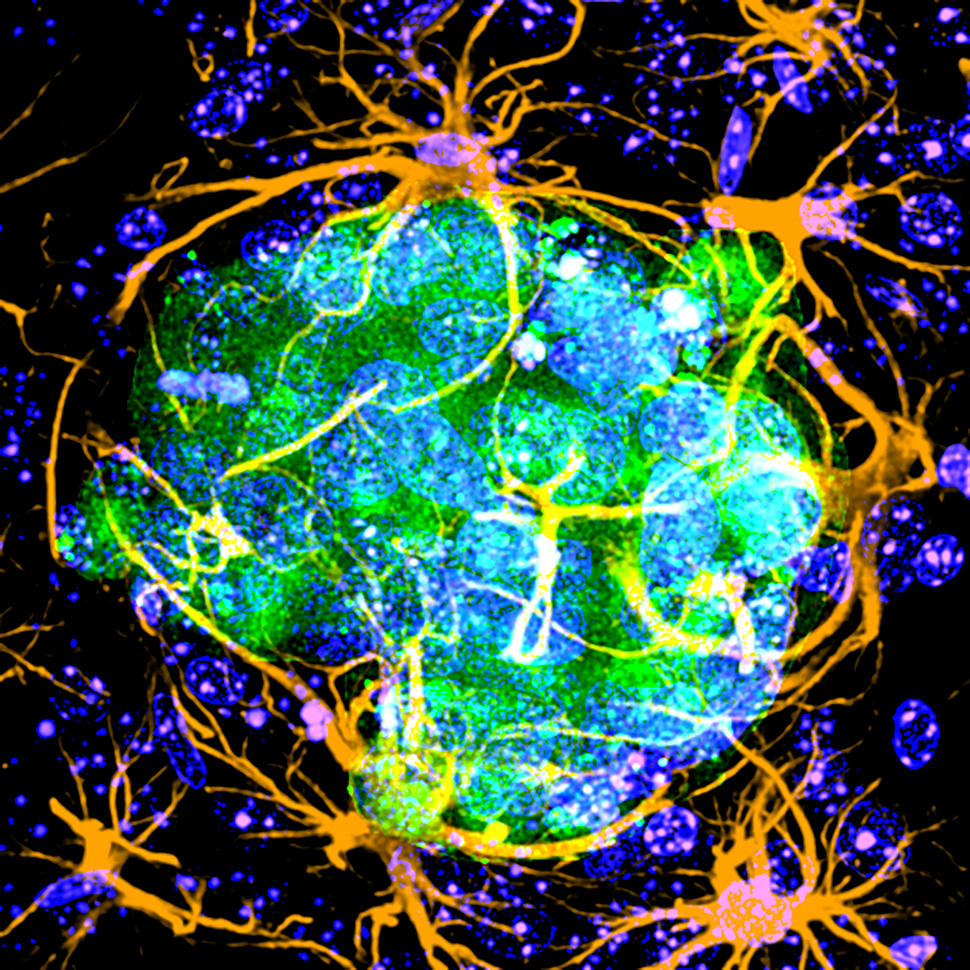
In mouse brains and in cultured cells taken from rat brains, Dr. Hernando-Monge and her team found that the amyloid beta produced by melanoma cells interacts directly with a type of brain cell called an astrocyte.
That interaction did several things, they found, including preventing immune cells in the brain called microglia from recognizing and killing the cancer cells.
Can Alzheimer’s drugs be repurposed to prevent brain metastases?
Taken together, these results raised the possibility that blocking amyloid beta could prevent melanoma from spreading to the brain.
So, in their final experiments, the researchers injected mice with human melanoma cells. Once tumors were established, they gave the mice a compound that blocks the generation of amyloid beta. As hoped, the compound helped reduce the formation of tumors in the brain.
This effect was seen regardless of whether the drug was given before or after the cells had already crossed the blood‒brain barrier.
The study only scratches the surface of understanding how cancer cells in the brain use amyloid beta, said Kevin Kleffman, a doctoral student in the Hernando-Monge lab who led the study. Melanoma cells may be exploiting a process involved in stopping long-term inflammation after a brain injury or some other process involved in repairing damaged brain cells.
Although more work is needed to understand the breadth of these interactions, Dr. Hernando-Monge stressed that there’s no direct link between melanoma and the development of Alzheimer’s disease.
“Alzheimer’s is associated with the accumulation of amyloid beta into plaques. We don’t see that in our melanoma models, and we don’t see that in patients [with melanoma],” she said.
But because amyloid beta has been the subject of intense interest in Alzheimer’s disease research, several drugs that block the protein have been developed as possible treatments for Alzheimer’s. These drugs have shown disappointing results in stopping or slowing Alzheimer’s itself. However, because they’ve proven very safe in large human studies, Dr. Hernando-Monge explained, they can easily be tested in human studies of other diseases.
Additional research would need to be done before trying such drugs in people with melanoma, the research team explained. Such studies include testing whether they would be safe in combination with the immunotherapy drugs that are now standard treatments for melanoma.
Eventually, the researchers hope to examine whether amyloid beta is needed for other types of cancer to spread to the brain, as well as for the growth of primary brain tumors such as glioblastoma.
Brain metastases can be devastating not only for people with melanoma, but for people with other cancers that tend to metastasize to the brain, including breast and lung cancer, said Dr. Hernando-Monge. “If amyloid beta is needed for other cancer types to spread to the brain, [this knowledge] could be applied to a larger set of patients.”
Additional research in this area may also help scientists better understand some aspects of neurodegenerative diseases, said Dr. Gril. “We often get the most insight from breaking down research silos between diseases and making connections between them.”