Cancer Immunotherapies Don’t Work for Everyone: HLA Gene May Explain Why
, by Nadia Jaber
Hundreds of thousands of people with cancer take immune checkpoint inhibitors, such as nivolumab (Opdivo) and pembrolizumab (Keytruda), every year. But for the majority of those people, the medicines—a type of immunotherapy—don’t work to treat their cancer.
Now NCI scientists think they’ve found a specific form of a gene that may make immune checkpoint inhibitors less effective for some people. The gene form, known as HLA-A*03, is found in 2% to 16% of the US population.
If the findings are confirmed in further studies, doctors could use the gene as a marker to help decide if a patient should or shouldn’t take an immune checkpoint inhibitor, said the scientist who led the study, Mary Carrington, Ph.D., of NCI's Center for Cancer Research.
That could spare many patients from getting treatments that don’t work for them and that can cause harsh side effects, Dr. Carrington added. But, she cautioned, “we need more data before [doctors would] actually use that [marker] in the clinic.”
In their analysis of data from thousands of patients, the researchers found that people with HLA-A*03 died sooner after immune checkpoint inhibitor treatment than people with other forms of the HLA-A gene. The study, published December 9 in Lancet Oncology, showed that this pattern held true for different immune checkpoint inhibitors and different types of cancer, including kidney, bladder, and skin cancer.
Timothy Chan, M.D., Ph.D., director of the Cleveland Clinic’s Center for Immunotherapy and Precision Immuno-Oncology, called the findings “exciting.” The next step, continued Dr. Chan, who was not involved in the study, is “to work out how [A*03] can be used most efficiently with other biomarkers” that are currently used to predict how well checkpoint inhibitors will work.
Different forms of HLA genes
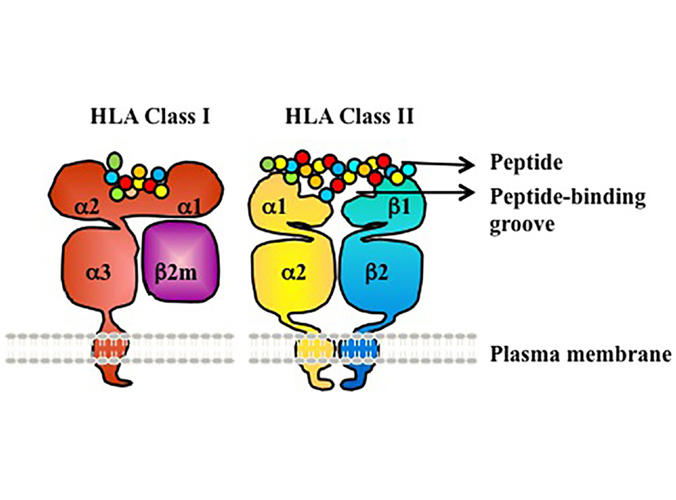
HLA-A is a member of a set of genes—including HLA-B and HLA-C—that help the immune system find and destroy cells that are cancerous or infected with a virus or bacteria.
These HLA genes make proteins called human leukocyte antigens (HLA), which take bits and pieces of proteins from inside the cell and display them on the cell’s surface. If the cell is cancerous or infected, the HLA proteins display abnormal fragments that trigger immune cells to destroy that cell and any others displaying the same fragment.
Across the human population, “there are thousands of different forms of these HLA genes, which we call alleles,” explained Dr. Carrington, who leads NCI’s HLA immunogenetics research.
A*03, for instance, is one of more than 2,000 alleles of HLA-A. That natural variation in HLA genes is, in part, what makes some people more susceptible than others to certain viral infections and autoimmune diseases.
Because immune checkpoint inhibitors help immune cells find and attack cancer cells, scientists have long suspected that variations in HLA genes may influence how well these treatments work.
Possible links between various HLA alleles and immune checkpoint inhibitor effectiveness have been studied extensively. But, so far, A*03 is the only one that seems to work as a marker of treatment response for multiple types of cancer and different immune checkpoint inhibitors, Dr. Carrington noted.
People with A*03 benefit less from immunotherapy
The team first sifted through data from a group of more than 1,000 people with 30 types of advanced cancer who were treated with an immune checkpoint inhibitor at Memorial Sloan Kettering Cancer Center.
Among various HLA alleles, HLA-A*03 emerged as the strongest biomarker of immune checkpoint inhibitor effectiveness. People with A*03, regardless of what kind of cancer they had, died nearly 1.5 times sooner after starting treatment than those with a different allele, the researchers found.
When the researchers separated the data by cancer type, A*03 was linked with a shorter time to death for people with bladder, brain (glioma), melanoma, lung, and kidney cancer. However, the impact of having A*03 was greatest in people with kidney cancer.
Among participants of four clinical studies who received an immune checkpoint inhibitor for kidney cancer, those with A*03 didn’t live as long before their kidney cancer grew back or they died (progression-free survival), compared with those who didn’t have the allele.
Confirming the findings in randomized clinical trials is very good evidence that A*03 is a biomarker of immune checkpoint inhibitor effectiveness, Dr. Chan noted.
Dr. Carrington and her team also found that people with two copies of A*03 died sooner than people with one copy of A*03 plus a copy of a different HLA-A allele (2.3 and 1.5 times sooner, respectively, than people with no copies of A*03).
The researchers validated their findings in two independent groups of patients who had been treated with immune checkpoint inhibitors—1,326 patients with various types of cancer treated at the Dana-Farber Cancer Institute and 169 people with bladder cancer who had participated in an international clinical trial. In both groups, those with A*03 died sooner after starting treatment than those without this form of the gene (1.2 and 1.4 times sooner, respectively).
The link between A*03 and immune checkpoint inhibitor effectiveness held true regardless of a person’s age, sex, ancestry, the type of immune checkpoint inhibitor they took, and whether they got chemotherapy at the same time. However, the allele wasn’t linked with the outcomes of other kinds of cancer treatment.
Combining biomarkers for immunotherapy
“While data from multiple clinical trials consistently showed the association of HLA-A*03 with less clinical benefit in patients treated with immunotherapy, these results should be validated in a prospective clinical study,” noted James Gulley, M.D., Ph.D., of NCI’s Center for Cancer Research and a leader of the study.
Testing for a specific HLA allele can be fast and reliable, the researchers noted. It’s done routinely to match donors and recipients for organ transplants, and as a way to tell who might have life-threatening allergic reactions to certain HIV and epilepsy treatments.
And HLA genes are included in several genetic biomarker tests that are commonly given to people with cancer, Dr. Chan noted.
But, Dr. Carrington cautioned, just because someone has A*03 doesn’t necessarily mean that they won’t benefit from immune checkpoint inhibitors.
In all of the data the researchers looked at, there were some people with A*03 for whom immune checkpoint inhibitor treatment worked. “It's when we look at the entire population of [people with] A*03 that we see, overall, there's less benefit,” she said.
Ultimately, models that combine multiple biomarkers might better predict whether an immune checkpoint inhibitor is likely to work for an individual, Dr. Chan said. “That's where this [field] is headed,” he added.
“Immunity is complex, and we know HLA is one part of the story,” he said. But many factors, from the total number of mutations in the tumor (tumor mutational burden) to the microbes that live in the gut, also influence how well immune checkpoint inhibitors work. And “it's clear that all these things work together,” Dr. Chan explained.
In a recent study, he and his colleagues built a model that takes into account a person’s genetics, biology, age, and tumor stage, among other factors, to predict whether checkpoint inhibitors are likely to work. The combination model was more accurate than tumor mutational burden alone at predicting whether a checkpoint inhibitor would be effective, the researchers found.
As for Dr. Carrington, her group is focused on understanding why immune checkpoint inhibitors don’t work well for people with A*03. They are currently sifting through several plausible explanations, but none has surfaced as the winner yet.
“We've been ruling things out one after another,” she said. But that’s the exciting part of science, she added, figuring out a great unknown.