Cabozantinib Approval Expands Initial Treatment Options for Advanced Kidney Cancer
, by Daryl McGrath
For patients with the most common type of kidney cancer, there is now a new approved use of the targeted therapy cabozantinib (Cabometyx®). In December 2017, the Food and Drug Administration (FDA) approved use of the drug as an initial, or first-line, treatment for patients with advanced renal cell carcinoma (RCC).
Cabozantinib was initially approved in 2016 for patients with metastatic RCC whose tumors did not respond to their first treatment or who had relapsed after previous treatment. (In 2012, a different formulation of the drug was approved under the trade name Cometriq® for the treatment of patients with medullary thyroid carcinoma.)
More than 60,000 people in the United States develop RCC each year. The overall incidence of kidney cancer has been increasing in the United States, while the mortality rate has decreased recently. Still, approximately 15,000 people in the United States are expected to die from this disease in 2018.
“Unfortunately, it’s a very lethal cancer,” said W. Marston Linehan, M.D., chief of the Urologic Oncology Branch in NCI’s Center for Cancer Research.
Over the last 13 years, however, FDA has approved numerous drugs, both targeted therapies and immunotherapies, to treat patients with various stages of RCC, Dr. Linehan pointed out.
“Patients now have a number of options to treat this aggressive disease,” he said.
A Deadly Silencing
The most common subtype of RCC, called clear cell RCC, accounts for 75% of cases. Ninety percent of clear cell RCC is caused by mutation or silencing of a gene called VHL, Dr. Linehan explained.
Twenty-five years ago, Dr. Linehan and his colleagues at NCI identified the VHL gene and demonstrated its critical role in kidney cancer. VHL is a tumor suppressor gene, and its silencing triggers a domino effect, resulting in the increased expression of genes and proteins that promote tumor cell survival and growth.
“Before we knew the genetic basis of this cancer, there were no effective therapies for patients with metastatic disease,” he said. As recently as 2005, “aside from Interleukin 2, very few targeted systemic therapies existed for metastatic RCC, and those that did were largely ineffective.”
But the past decade or so has seen an encouraging increase in the number of drugs targeting the underlying genetic mechanisms of kidney cancer, he continued.
“We now have numerous drugs, including cabozantinib, targeting the VHL pathway that are FDA approved for patients with advanced kidney cancer,” Dr. Linehan said.
Cabozantinib Delays Cancer Growth
The new approval of cabozantinib was based on data from an NCI-sponsored randomized phase 2 trial in which 157 patients with metastatic kidney cancer were randomly assigned to receive either cabozantinib or sunitinib (Sutent®), a drug commonly used as first-line treatment for advanced RCC. Both drugs are pills taken by mouth.
The trial, called CABOSUN, compared each drug’s ability to prevent RCC from worsening, an outcome called progression-free survival. Patients treated with cabozantinib had a median progression-free survival of 8.6 months, compared with 5.3 months for patients taking sunitinib.
Patients taking cabozantinib were also more likely to respond to treatment, with 33% having a partial or complete response compared with 12% for those taking sunitinib. Those taking cabozantinib were also more likely than those taking sunitinib to have stable disease as a best response: 46% versus 42%.
Manageable Side Effects
Almost all patients in the trial experienced side effects and, in about two-thirds of them, those side effects were considered serious. The most common serious side effects experienced by patients treated with cabozantinib included diarrhea, high blood pressure, and hand-foot syndrome. Other side effects included fatigue, nausea, decreased appetite, and painful mouth sores.
There were three treatment-related deaths in each arm of the trial. Dose reductions were more common in patients treated with cabozantinib, but the rate of treatment discontinuation was the same, with about 20% of patients in each arm stopping treatment because of side effects.
Despite the prevalence of adverse events, the side effects of cabozantinib are comparable to other drugs in this class, said Dr. Linehan, “and they are manageable.”
That perspective is supported by the recent publication of quality of life results from the phase 3 METEOR trial that formed the basis for cabozantinib’s initial approval for RCC in 2016. Patients in that trial experienced a similar quality of life and a longer period before deterioration of quality of life compared to patients treated with everolimus (Afinitor®).
Drugs Block Blood Vessel Growth
Cabozantinib and sunitinib are members of a group of drugs called tyrosine kinase inhibitors (TKIs), which block the action of various proteins involved in cell signaling, growth, and division.
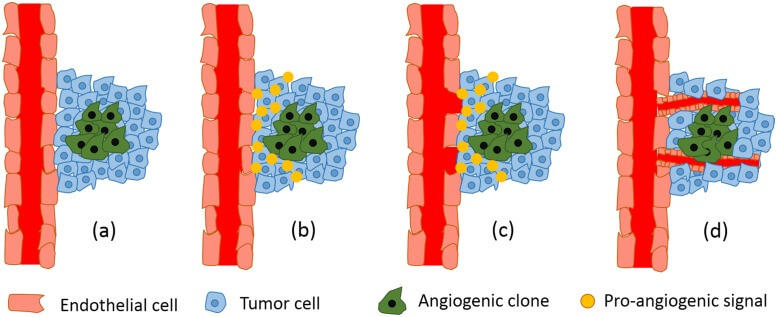
Both drugs block a protein called VEGF that promotes angiogenesis, the formation of new blood vessels that feed the growth of tumors. The VEGF gene is part of the genetic pathway activated by the mutated VHL gene that leads to RCC. To date, FDA has approved nine angiogenesis inhibitors for patients with kidney cancer, although not all are TKIs.
“The approval of cabozantinib provides another option for patients and doctors,” said Brian Rini, M.D., a kidney cancer expert at the Cleveland Clinic Taussig Cancer Institute.
Although all the drugs block angiogenesis, he pointed out, they are not identical. They may inhibit their targets in different ways, or they may inhibit different molecular targets. All the TKIs approved for RCC inhibit VEGF, but cabozantinib also inhibits several other gene pathways that are important in kidney cancer development.
“There may be good and bad in that,” Dr. Rini said. Some drugs may have “better clinical activity for some patients, but there may also be additional toxicity” caused by inhibiting those pathways. “There are good and bad characteristics of each one, so it’s always good to have more options,” he said.
One benefit of having more options is that it allows doctors to address a common problem with anti-angiogenesis therapy: drug resistance. In most patients, tumors treated with VEGF-targeted agents eventually develop resistance to the drugs, and the disease then progresses.
However, “it’s very common for doctors treating patients with advanced kidney cancer to start with one agent and then, if the treatment is no longer benefiting the patient, to switch to another agent or add an agent to the regimen,” explained Dr. Linehan.
Combination Therapies: The Future of Kidney Cancer Treatment?
While the approval of cabozantinib adds another TKI to the available options for patients with advanced kidney cancer, combination therapy involving TKIs and other agents is likely to be the future for these patients, according to Dr. Rini.
“There are a lot of trials of drug combinations that are beginning to report results,” Dr. Rini said. “We expect this whole landscape is going to change in the next year or so. We won’t be giving single TKIs to patients with metastatic RCC as front-line therapy for very long.”
Dr. Linehan echoed Dr. Rini’s prediction.
“There is a lot of excitement about the potential of combining immunologic agents with these targeted TKIs,” he said.