Drug Combination Reduces Number of Colorectal Polyps in Patients with Hereditary Cancer Syndrome
, by NCI Staff
In a new analysis of a prevention clinical trial, a two-drug combination substantially decreased the number of precancerous colorectal polyps in people with a very high hereditary risk of developing colorectal cancer.
In the trial, people with this hereditary condition—called familial adenomatous polyposis (FAP)—who were randomly assigned to receive the combination of erlotinib (Tarceva) and sulindac (Aflodac) had less than a third the number of polyps after 6 months of treatment than patients who received placebos. The new analysis was published February 8 in JAMA Oncology.
Earlier results from the same randomized clinical trial showed that treatment with these two drugs decreased the number of polyps in the duodenum (the first part of the small intestine) by about 70%. Reduction in duodenal polyps was the primary goal of the trial. However, the researchers had also planned to look at colorectal polyp reduction as a secondary endpoint.
The initial results were "remarkable, as no other drug has shown efficacy in reducing duodenal polyp burden," commented Asad Umar, D.V.M., Ph.D., chief of the Gastrointestinal and Other Cancers Research Group in NCI's Division of Cancer Prevention. "The new analysis shows that the combination has a potential cancer preventive effect on colorectal polyps, as well."
However, Dr. Umar cautioned, whether the two drugs together work dramatically better than either one alone in those with FAP cannot be determined from this trial, since it only tested the combination.
And while the results are exciting, many questions about chemoprevention in people with FAP remain unanswered, explained Jewel Samadder, M.D., of the Mayo Clinic in Phoenix, Arizona, who led the trial.
"But the goal, we hope, is that ultimately we can come up with a chemopreventive regimen that will markedly reduce the risk of cancer in patients with FAP," said Dr. Samadder.
Targeting Aggressive Cell Growth
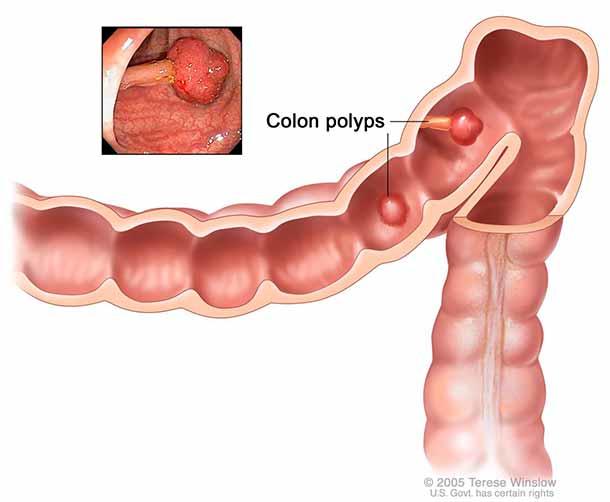
People with FAP have an inherited mutation in a gene called APC, which normally is involved in suppressing cell growth in the digestive tract. Mutations in APC disrupt its activity, which can lead to the formation of hundreds to thousands of polyps during a person’s lifetime.
People with FAP have a nearly 100% risk that such polyps will progress to colorectal cancer, and up to 12% of FAP patients also develop duodenal cancer.
Consequently, people with FAP undergo regular endoscopic monitoring and polyp removal. But when the number of polyps in the colon and rectum becomes too great to control in this way, they typically have a colectomy—the removal of all or part of the colon. Although this procedure almost completely reduces the risk of colorectal cancer, it can have a dramatic effect on a person's quality of life, explained Dr. Samadder.
In addition, duodenal cancer is much harder to prevent or treat surgically, he continued, which is why the main goal of the trial was to see if the two-drug combination reduced the burden of duodenal polyps in patients with FAP.
Much has been learned about how APC mutations lead to the development of gastrointestinal polyps. Two of the proteins involved in this process, EGFR and COX2, can be blocked with existing drugs, and researchers have long suggested that combining drugs that target both proteins might reduce polyp formation.
In the current trial, erlotinib—an EGFR inhibitor that is already used to treat lung and pancreatic cancer—was combined with sulindac, which targets COX2.
Major Reduction in Polyp Number
The trial enrolled 92 people with FAP beginning in 2010. The participants were randomly assigned to receive daily treatment with either erlotinib and sulindac pills or two identical-looking placebo pills. The number of polyps in both the duodenum and colorectum were measured using endoscopy before and after 6 months of treatment.
After the first 67 participants had finished 6 months of treatment, the trial's Data and Safety Monitoring Board recommended stopping enrollment, due to the dramatic reduction in duodenal polyps seen in the patients who had received erlotinib and sulindac.
During follow-up, patients who had received 6 months of erlotinib and sulindac also experienced a net drop of approximately 70% in the number of colorectal polyps from the start of the study, compared with the placebo group.
This effect was observed even though almost three-quarters of the patients given the two drugs had to have their dose of erlotinib reduced because of side effects, most often a painful rash. About half of participants receiving the two drugs also had a reduction in sulindac dose, for side effects including nausea and diarrhea.
There was no correlation between the total amount of either drug taken and the reduction in colorectal polyp burden—which, the trial leaders believe, suggests that the doses chosen were more than enough to interfere with the harmful molecular signaling in patients with FAP.
Future Questions
Unanswered questions about using such a drug regimen widely in people with FAP include whether it can reduce the number of duodenal and colorectal polyps long-term, as well as reduce the risk of polyps progressing to cancer. The researchers would also like to know if the drugs can reduce the need for colectomy in people with FAP, said Dr. Samadder.
In addition, they want to explore whether chemopreventive drugs for duodenal or colorectal cancer have to be taken continuously, or whether they could be taken intermittently to reduce the side effect and cost burden on patients.
And if preventive drugs need to be taken for a long period of time, the types and amount of the drugs would likely have to be tweaked, Dr. Samadder explained, because some people cannot tolerate the side effects of erlotinib. The research team is currently enrolling patients into a new trial that is looking at whether a reduced dose of erlotinib alone, given less often, would be as effective but less toxic than the combination used in this trial.
"We're not treating cancer, we're trying to prevent it, so you need to have a drug [regimen] that's highly tolerable," said Dr. Samadder.
It would also be interesting to test lower doses of both drugs in combination, commented Jason Zell, D.O., from the University of California, Irvine, who is working on a different clinical trial of colorectal cancer chemoprevention.
"If there is a lower effective dose of erlotinib that would work synergistically with sulindac in this population and would give similar efficacy results, that would be outstanding," he commented.
Preventing High-Risk Adenomas and Second Cancers in Colorectal Cancer Survivors
There is growing interest in testing drugs to prevent the development of high-risk precancers (called adenomas) or a second primary colorectal cancer in people who have already been treated for the disease.
People who have been treated successfully for colorectal cancer are at higher risk of developing adenomas or a new colorectal cancer than the general population. But because their risk is much lower than that of people with FAP, a chemoprevention regimen would have to come with very few side effects to have any appeal, explained Dr. Zell, who is leading a chemoprevention clinical trial in colorectal cancer survivors called PACES.
That trial, sponsored by NCI's Division of Cancer Prevention and open at more than 500 hospitals across the country, is enrolling patients who have been treated within the previous year for localized colorectal cancer. Participants are being randomly assigned to one of four groups: a combination of sulindac and eflornithine; sulindac plus a placebo; eflornithine plus a placebo; or two placebos.
Eflornithine inhibits the activity of a class of enzymes known as polyamines, which may promote cancer formation in the colon and rectum, explained Dr. Zell. Sulindac, in addition to targeting COX2, also inhibits polyamine activity. Participants will take their pills for 3 years and be followed by the researchers for a total of 8 years. The hope is that one or both drugs will reduce the risk of adenomas and second primary colorectal cancers by about half during that time, Dr. Zell said.