Immunotherapy’s Skin Side Effects: Are Microbes to Blame?
, by Elia Ben-Ari
Drugs called immune checkpoint inhibitors are a type of immunotherapy that have transformed the treatment of many cancers. But for many patients, these drugs can cause a wide range of side effects, including itching and painful skin rashes. Sometimes, the skin side effects are bad enough that people stop taking the drugs.
A new study in mice suggests that the skin side effects may occur because the drugs cause the immune system to attack new microbes that take up residence on the skin. If confirmed in humans, this insight could ultimately lead to better ways to treat or prevent the skin complications of immune checkpoint inhibitor treatment.
The findings suggest that these skin side effects may be triggered by new additions to the communities of bacteria, fungi, and other microbes that live in and on us, collectively known as the microbiota, said Yasmine Belkaid, Ph.D., of the National Institute of Allergy and Infectious Diseases (NIAID), one of the study’s senior investigators. People are exposed to new types of microbes all the time, especially in hospitals, Dr. Belkaid said.
Immune checkpoint inhibitors take the brakes off cancer-killing immune cells. But these activated immune cells can also harm healthy cells and tissues, leading to inflammation and immune-related side effects. The mechanisms underlying these side effects, which are often treated with steroid drugs, are not clear.
The study results “open up a new way of thinking” about skin side effects and possibly also other inflammatory side effects, but will need to be verified in human studies, said immunotherapy expert James Gulley, M.D., Ph.D., of NCI’s Center for Cancer Research, who was not involved in the study.
Microbes and the immune system: constant communication
“The immune system is constantly communicating with the skin microbiota,” Dr. Belkaid said. This two-way dialogue can prevent harmful immune reactions and inflammation when the immune system encounters a new type of microbe on the skin that doesn’t pose a threat.
“Mouse studies suggest that the skin microbiome helps ‘educate’ the immune system” to distinguish dangerous pathogens from beneficial or harmless microbes, explained dermatologist Heidi Kong, M.D., M.H.Sc., of the National Institute of Arthritis and Musculoskeletal and Skin Diseases, who was not involved in the new work.
Studies in mice by Dr. Belkaid’s lab and others have also shown that some interactions between microbes and the immune system promote wound healing and protect against infection. But under some circumstances, these interactions can turn harmful.
The role of the skin microbiota in people is not as easy to study as it is in mice because exposures to skin bacteria are easier to control in mouse studies, said Dr. Kong. But it’s clear that “if our skin were to have an inflammatory response to everything that it came into contact with, including new microbes, we’d be walking around constantly inflamed,” she said.
Immune checkpoint inhibitors disturb the peace
Dr. Belkaid’s team wondered whether the skin side effects of immune checkpoint inhibitors might be a consequence of the drug disrupting the normal dialogue between the skin microbiota and the immune system.
They began by treating lab mice with the immune checkpoint inhibitor ipilimumab (Yervoy) and applying Staphylococcus epidermidis bacteria to the skin of these mice at the same time.
Although S. epidermidis is not normally found on mice, previous work by Dr. Belkaid’s lab showed that these microbes can easily take up residence on the skin of mice “and become a lifelong partner,” she said.
Mice simultaneously treated with ipilimumab and exposed to S. epidermidis developed “striking skin inflammation,” the study team wrote. By contrast, when used on their own, these treatments did not result in inflammation.
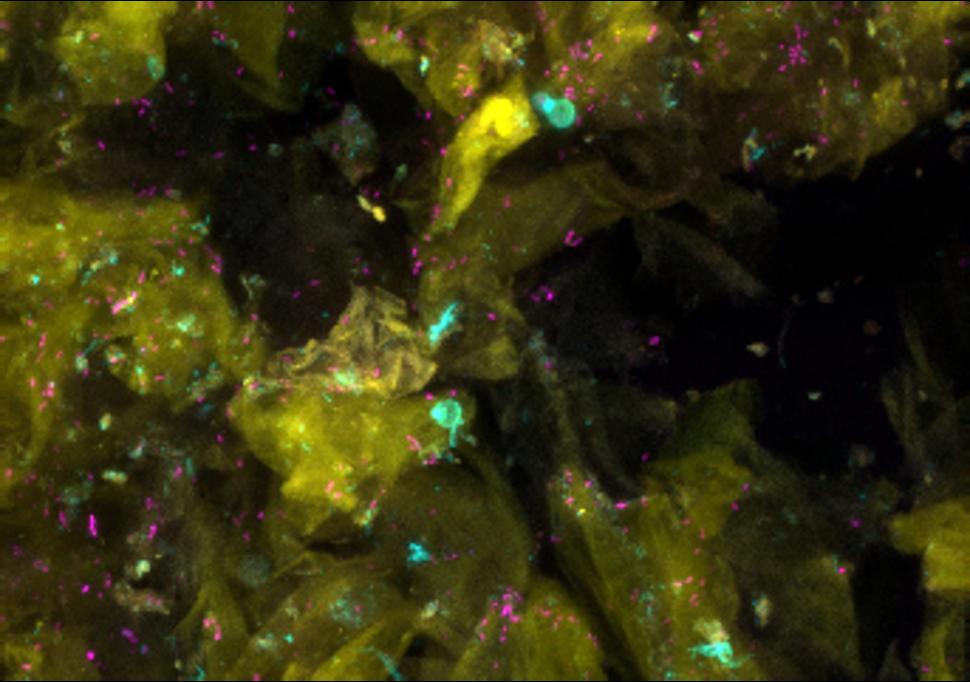
The inflamed mouse skin contained elevated levels of T cells, the team found. These T cells, which specifically targeted S. epidermidis, produced a substance called IL-17 that can promote inflammation. Additional experiments indicated that excessive IL-17 secreted by the T cells was driving skin inflammation in the mice.
Because the skin side effects of immune checkpoint inhibitors in patients may not appear until after treatment ends, the team also looked at the long-term consequences of immune checkpoint inhibitor treatment.
They found that, compared with their response to the initial exposure to S. epidermidis, mice that had been treated with ipilimumab had a stronger and more rapid inflammatory response to S. epidermidis when they were re-exposed to the bacteria a month after the initial exposure.
These re-exposed mice also had increased numbers of memory T cells directed against the bacteria. Memory T cells can linger in the body to be quickly called up if a threat reappears. The researchers concluded that immune checkpoint inhibitor treatment may lead to long-term abnormal memory T-cell responses in mice encountering the same microbe again, even months after treatment with the drug has ended.
Microbes cause pendulum to swing toward excess inflammation
“Our study shows that, in mice, the peaceful relationship between the microbiota and the immune system can be profoundly affected” by treatment with an immune checkpoint inhibitor, Dr. Belkaid said.
It raises the possibility that exposure to new microorganisms in the skin and other parts of the body, such as the gut, may lead to inflammation if checkpoint inhibitor treatment is started around the same time, Dr. Gulley said.
“It’s intriguing to see how, in this mouse model, you can cause the pendulum to swing toward too much inflammation” in response to the skin microbiota, Dr. Kong said. It would be interesting to see if the same effects occur in wild mice, whose immune systems are more similar to the human immune system, she added.
Ultimately, Dr. Belkaid emphasized, studies in patients treated with immune checkpoint inhibitors are needed to see if these findings in mice reflect what happens in humans. The study’s lead investigator, Z. Ian Hu, M.D., Ph.D., a former NCI clinical research fellow who is now at Washington University in St. Louis, hopes to pursue such research.
For instance, the team wrote, future studies could look at the composition of the skin microbiota in patients before and during immune checkpoint inhibitor treatment to find out how changes in the microbiota influence the severity and development of skin side effects.
“This study opens up a new series of questions that can form testable hypotheses,” Dr. Gulley said.
Another important question is whether the results apply to immune-related side effects of checkpoint inhibitors in other organs besides skin, such as inflammation of the colon (colitis), which is more serious than most skin side effects seen with the drugs.
It also remains to be seen whether similar effects are seen with other commonly used immune checkpoint inhibitors, such as pembrolizumab (Keytruda) and atezolizumab (Tecentriq), which have different molecular targets than ipilimumab.
If the effects of immune checkpoint inhibition that Dr. Belkaid’s team observed in mice also occur in humans, Dr. Gulley said, it may be possible to prevent or treat immune-related side effects of checkpoint inhibitors by blocking the effects of IL-17. A medication that blocks IL-17 is already used to treat psoriasis and some types of arthritis.
Finally, he said, another question is whether ensuring that people have a diverse microbiota before starting checkpoint inhibitor therapy could reduce the risk of immune-related side effects by lessening the chances of acquiring new microbes. Studies suggest that exercising or eating a high-fiber diet, for example, can increase the diversity of the microbiota.